HIGHLIGHTS
Novel Deep Brain Stimulation Approach Shows Early Promise for Aphasia Treatment Development
Led by Emad N. Eskandar, MD, MBA, Chair of Neurological Surgery, and Nathaniel J. Killian, PhD, Assistant Professor of Neurological Surgery, researchers at Montefiore Einstein report early evidence from a first-in-human pilot study that appropriately timed striatal deep brain stimulation can accelerate language learning, increase proficiency and enhance long-term retention of novel words. These data were presented at the Society for Neuroscience meeting, held in San Diego in November 2025. The findings provide proof of principle that targeted neuromodulation of striatal learning circuits, including the nucleus accumbens (NAc) and caudate (Cd) nucleus, may offer a promising new direction for aphasia treatment development.
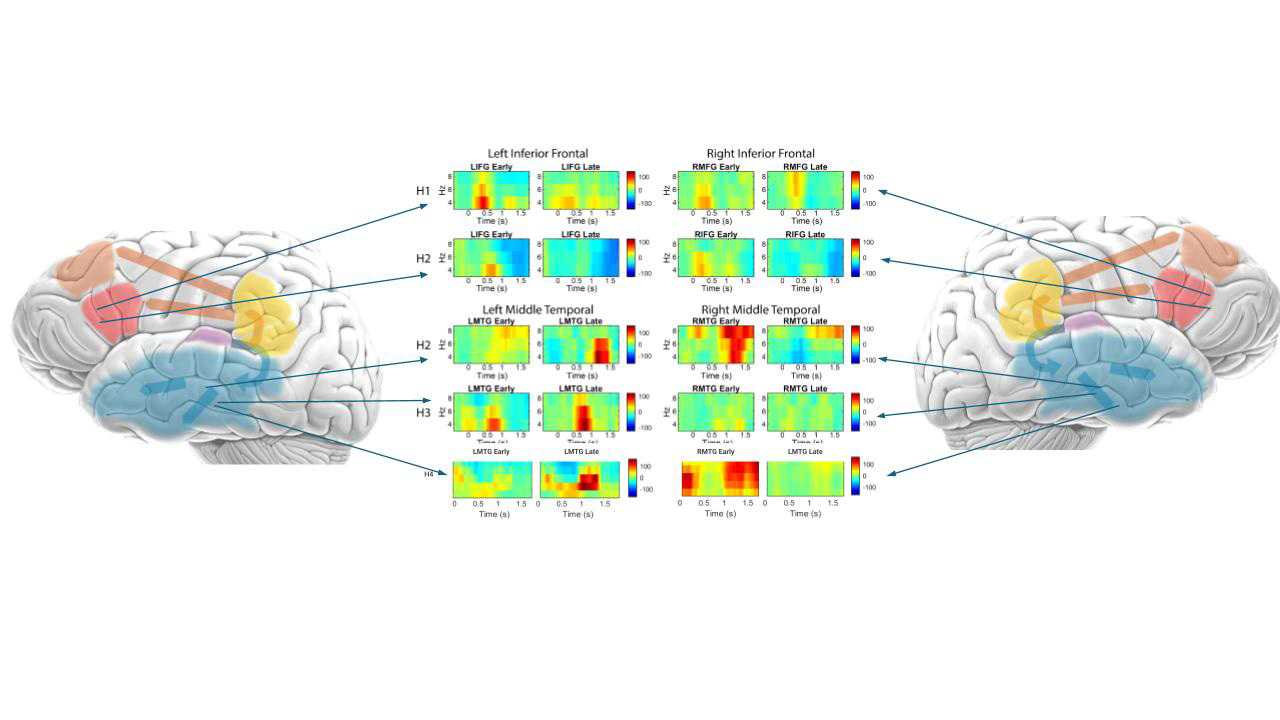
In this pilot human study involving epilepsy patients implanted with depth electrodes, researchers evaluated the effects of timed striatal stimulation during a language-learning task. Participants were asked to learn word-meaning associations from an unfamiliar language, Swahili. For half of the words, stimulation was delivered to the NAc at word presentation and to the Cd following correct responses, while the remaining words served as unstimulated controls.
Across participants, stimulation was associated with higher learning rates, greater proficiency and enhanced long-term retention, roughly halving the number of trials needed to learn novel words. In one participant with baseline language impairment, the median number of trials required to reach criterion decreased from 24 to 6, an approximate 75% reduction. While preliminary, these findings demonstrate proof of principle that appropriately timed striatal stimulation can enhance language learning, particularly in individuals with language impairments, and could ultimately inform strategies to support accelerated recovery in patients with aphasia.
Unlike noninvasive neuromodulation techniques such as transcranial magnetic stimulation (TMS) or transcranial direct current stimulation (tDCS), or peripheral approaches such as vagus nerve stimulation (VNS), this strategy directly targets deep striatal learning circuits. It delivers precisely timed stimulation during active language learning, providing a biological and mechanistic foundation for a novel approach to aphasia treatment development.
“These early findings suggest that appropriately timed striatal deep brain stimulation can significantly enhance language learning, particularly in patients with language impairments,” said Dr. Eskandar. “While preliminary, the results offer encouraging early evidence that targeted neuromodulation could help inform future therapeutic strategies for individuals with aphasia who currently have limited treatment options.”
The study builds on extensive prior research demonstrating that combined NAc and Cd stimulation enhances learning in primate models, produces near-complete recovery from brain injury in rodent models and accelerates acquisition of abstract associations in humans. Three complementary biological mechanisms have been identified: induced phasic dopamine release, increased neurite outgrowth and enhanced synaptogenesis.
Together, these findings establish a scientific foundation supporting a framework that reconceptualizes aphasia, and potentially other neuropsychiatric conditions, as impairments in learning. Ongoing research initiatives are advancing the development and testing of a neuromodulation-based brain-computer interface that pairs implantable stimulation targeting corticostriatal structures critical for language learning with an adaptive, artificial intelligence-based language therapy application designed to precisely trigger stimulation of the NAc or Cd. This approach aims to harness neuroplasticity through appropriately timed neuromodulation to inform future aphasia treatment strategies.
Aphasia is a language disorder characterized by impaired speech production and comprehension that affects an estimated 2.5 million Americans and represents a major source of long-term disability and unmet clinical need. Most commonly caused by left-hemisphere stroke, but also by traumatic brain injury, brain tumors, neurosurgery or neurodegenerative disease, aphasia occurs in approximately 30 to 40 percent of stroke survivors, with nearly half experiencing persistent impairment. Despite its profound impact on communication, independence and quality of life, treatment options remain limited. Speech and language therapy is the mainstay of care, yet recovery is highly variable and often modest, particularly in chronic moderate-to-severe aphasia, for which no effective medical or surgical treatments currently exist. Individuals with aphasia experience significantly higher rates of depression and disability, and in a study of more than 66,000 individuals, aphasia was shown to have the greatest negative impact on quality of life among 15 major illnesses, including cancer and Alzheimer’s disease.
This work highlights Montefiore Einstein’s leadership and commitment to pioneering translational neurosurgical approaches and innovative therapies aimed at improving outcomes and quality of life for patients with complex neurologic conditions. As the first health system from the Bronx to the Hudson Valley to earn Comprehensive Stroke Center designation from The Joint Commission and one of the first Comprehensive Level 4 Epilepsy Centers, Montefiore Einstein is ranked in the top 1 percent of all hospitals in the nation for neurology and neurosurgery, according to U.S. News & World Report.
Patient referrals
At Montefiore Einstein Neurosurgery, we know providing patients with the best possible care includes teamwork and trust. We work closely with our valued referring physicians to ensure open communication and reliable expertise.
Contact Us
Emad Eskandar MD, MBA,
David B. Keidan Professor and Chair of Neurological Surgery
eli@montefiore.org