HIGHLIGHTS
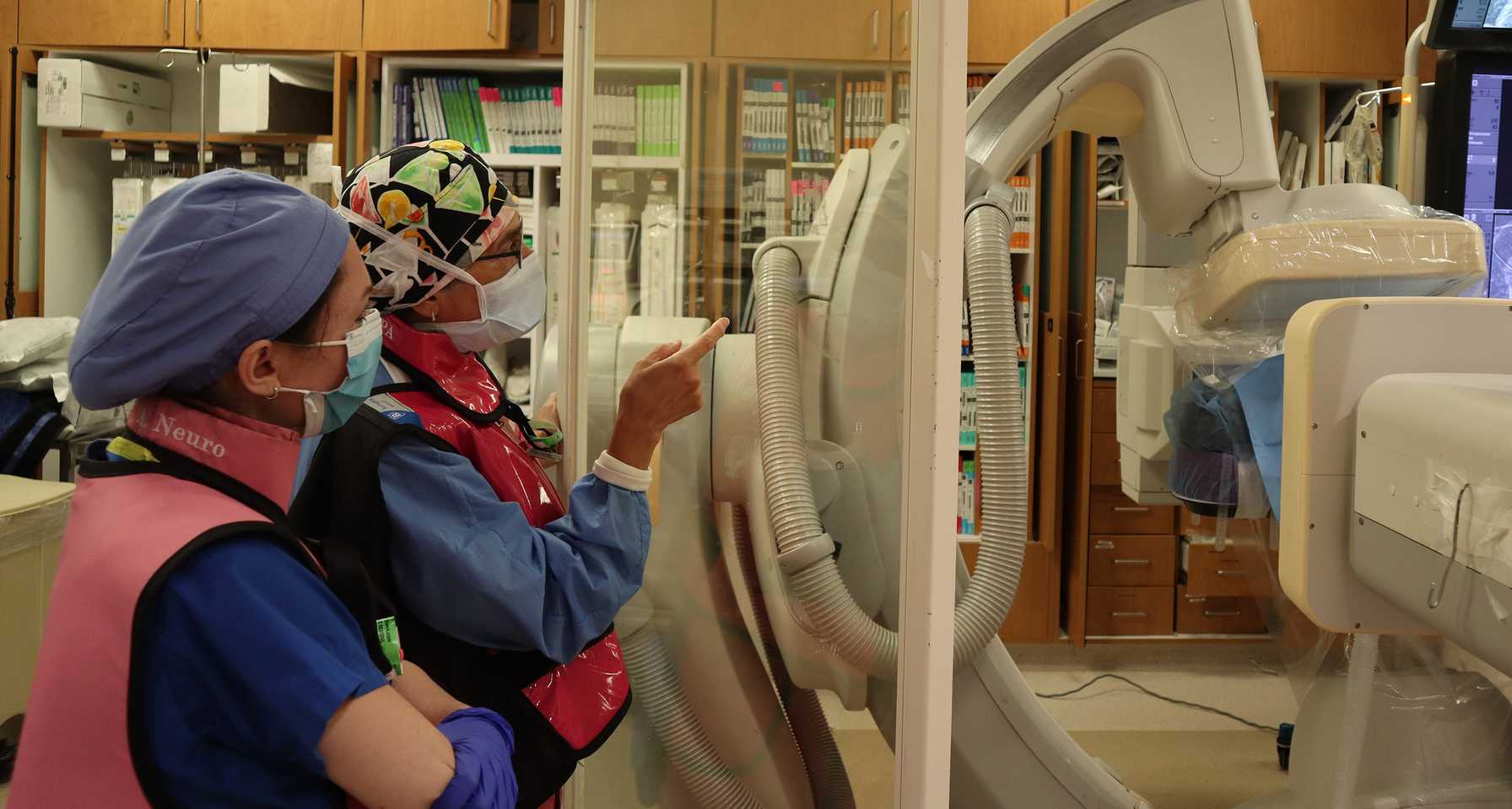
Department of Anesthesiology Expands Services Outside OR to Augment Patient-Centered Care
Across all Montefiore Medical Center campuses, there were more than 23,526 NORA procedures performed in 2023 – up from 19,935 procedures in 2022. The majority of these procedures take place at the Moses Campus, where Dr. Curtis Choice has served as Anesthesia Site Director since 2020. Dr. Choice said the expansion of NORA services at Moses arose from an increased demand from specialties across the health system, which are performing a larger number of non-invasive procedures outside the OR for diagnostic and therapeutic purposes. These procedures typically do not require general anesthesia, Dr. Choice explained, but rather the anesthesia provider utilizes a sedative medication.
To meet the increased demand, Dr. Choice, NORA Director Dr. Irene Osborn, and Moses Associate Site Directors Drs. Adela Aguirre-Alarcon and Michael Rufino have worked to create a system that allows the anesthesiology team to respond to requests for NORA procedures in an organized, timely fashion. As Dr. Choice recently began his new role as Senior Director of Network Integration and Expansion, new Moses Anesthesia Site Director Dr. Arthur Hertling has assumed the position and is overseeing collaborations between Anesthesiology and non-OR services.
"Our goal is that every patient who requires sedation or general anesthesia for a procedure outside of the operating room is able to receive it safely and in a timely manner,” Dr. Hertling said.
Dr. Aguirre-Alarcon noted that although NORA procedures are minimally invasive, many of the procedures are complex for patients who are typically very sick. She described, for example, a procedure she was involved in recently in which a teenage patient undergoing intrathecal chemotherapy required a percutaneous transhepatic cholangiogram (PTC), or a drain put into the hepatic system to relieve blockage.
Drs. Aguirre-Alarcon and Choice noted that for patients who have complicated conditions as well as those who are more vulnerable such as the elderly, conducting minimally invasive procedures instead of invasive surgeries is preferred.
“There’s a shift to trying to do things as minimally as possible,” Dr. Choice explained. “If it means a lower risk to the older, frailer patient, there are plenty of procedures that were previously done surgically but are now done through interventional radiology like the insertion of different drains and vascular access.”
Dr. Osborn, who was appointed Director of NORA Services in October 2022, explained that multidisciplinary collaboration is an essential part of coordinating the NORA schedule. Dr. Osborn regularly works with the Department of Radiology to coordinate magnetic resonance imaging (MRI) tests for patients who are unable to undergo the test without sedation due to anxiety or pain.
“As anesthesia providers, we bring safety and we bring the ability to keep the patient still,” Dr. Osborn said. “For certain procedures, this is essential because if the patient moves something devastating could happen."
Dr. Osborn previously served as the Neuroanesthesia Division Director and said her interest in NORA procedures began when she started working on neurointerventional radiology cases when she worked at New York University Langone and Mount Sinai prior to Montefiore. She explained that interventional radiology was an exciting field when it was introduced because instead of clipping aneurisms, neurosurgeons were able to utilize coiling, which is much less invasive. Dr. Osborn has continued to use her expertise to help patients and collaborate with other services such as the Gynecology Oncology group and the Department of Radiation Oncology. Together with interdisciplinary colleagues, Dr. Osborn has developed a process for managing these patients utilizing deep sedation during their radiation treatments.
“One of the things about NORA is you have a chance as an anesthesia provider to interact with so many other medical professionals and help a variety of patients,” Dr. Osborn said. "For the radiation oncology patients, it makes the difference in patients getting their treatment and hopefully prolonging their lives.”
This year, the Department of Anesthesiology will expand services within both Cardiology and Gastroenterology to continue to elevate the quality of care. NORA procedures performed by gastroenterologists take place in the endoscopic suite and range from diagnostic procedures to advanced endoscopic procedures. Dr. Oleg Evgenov recently started at Montefiore Einstein as the new Division Director of Endoscopic Anesthesia and Advanced Endoscopic Anesthesia. He said there are approximately 1,350 endoscopic procedures performed across the Moses, Wakefield, and Weiler campuses each month. Because of this high volume as well as the serious illnesses many of the patients face, Dr. Evgenov emphasized the importance of multidisciplinary collaboration.
“Within the last few months, we have worked on several process improvement projects that have a big impact,” Dr. Evgenov said. “This includes having additional equipment and medication readily available in the procedure rooms to improve our time management between cases."
For Department of Anesthesiology Chair Dr. Matthias Eikermann, ensuring that anesthesia providers are available for all patients requiring NORA services is a top priority. In addition to greater collaboration and efficiency, having an anesthesiologist administer sedation in NORA settings has been shown to improve patient outcomes.
Building upon the body of literature in this area, Dr. Eikermann and his team of researchers in the Anesthesiology Digital Health Lab have been conducting a retrospective, observational study of Montefiore Einstein patients who underwent an interventional radiology or gastroenterology procedure between 2016 and 2022.
The researchers studied data from more than 22,800 patients and found that for patients who received sedation from an anesthesiologist for NORA procedures, there was a 44-percent reduced risk of non-home discharge. The team found that patients undergoing biliary or vascular procedures, as well as those who were admitted to the ICU within 72 hours prior to their procedure, benefit the most from having an anesthesiologist manage their sedation.
“Based on our data, we speculate that the rigorous training needed to become an anesthesiologist helps us identify critically ill patients who need advanced care in the ICU, for example,” Dr. Eikermann explained. “This identification then minimizes the risk of ‘failure to rescue.’”
Patient referrals
At Montefiore Einstein Anesthesiology, we know providing patients with the best possible care includes teamwork and trust. We work closely with our valued referring physicians to ensure open communication and reliable expertise.